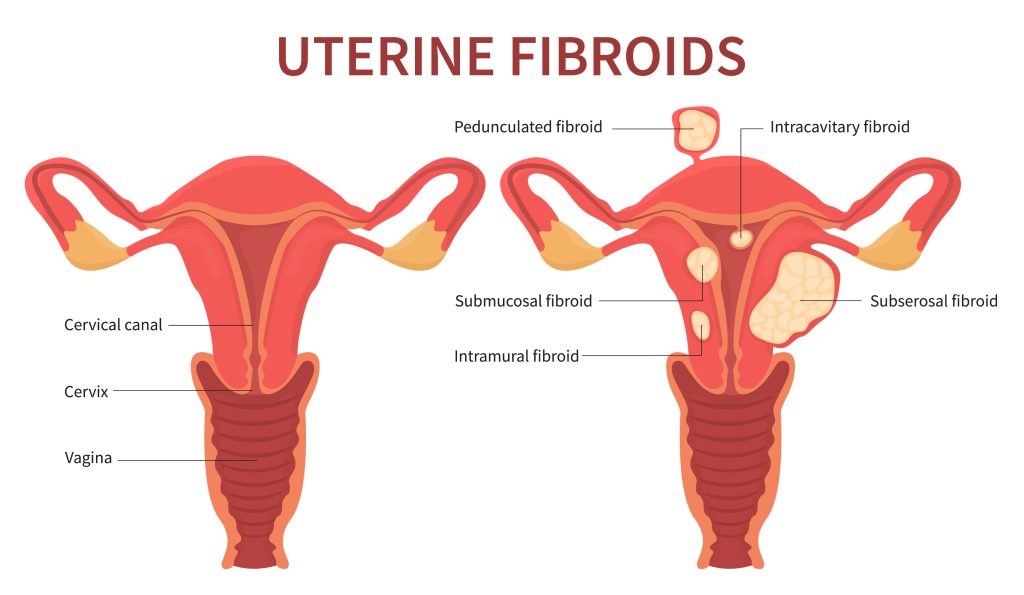
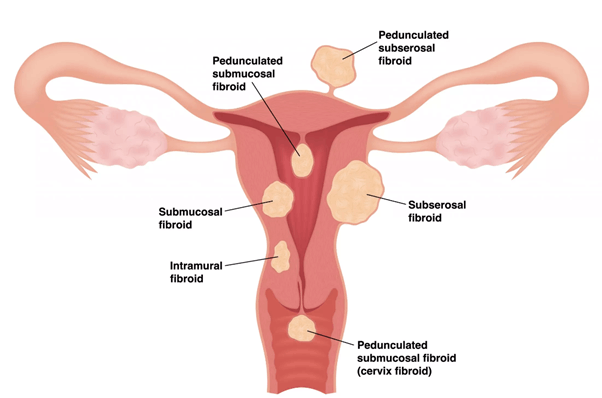
Fibroids or uterine leiomyomas are benign, noncancerous growths inside the uterus or in its muscular wall. Fibroids can vary enormously in size, from that of a pea to that of a melon. Between 20% and 40% of women over 35 years of age have fibroids. Multiple growths may be present at the same time, anywhere in the uterus. They are classified according to their location:
What are the most common symtoms?
Symptoms vary, but most common symptoms are:
- regular, heavy menstrual bleeding
- pain in the pelvic area
- heaviness, cramps and swelling of the abdomen
- pain during urination or bowel movement
- infertility
Such symptoms do not necessarily mean that fibroids are present, which can only be confirmed by pelvic examination, possibly including an ultrasound scan or a magnetic resonance imaging (MRI) examination.
Most fibroids are asymptomatic and do not cause any particular problem. If this is the case, treatment is unnecessary.
"Embolisation preserves the uterus and is an alternative to surgical removal."
THREE TYPES OF TREATMENT
Drugs: antihemorrhagic or anti-inflammatories can be used to treat the patient's symptoms. Certain hormones can also be beneficial. However, the efficacy of drugs and hormones is usually limited and their effects are temporary. Moreover, side effects may limit the duration of the course of treatment.
Surgical removal: various surgical techniques can be used, depending on the size, number and location of the fibroids: Myomectomy involves the individual removal of each leiomyoma. Different approaches can be used, including coelioscopy, hysteroscopy or abdominal incision, but all entail a hospital stay of several days followed by a one to six week convalescence period.
Myomectomy can complicate subsequent pregnancies because it causes scarring of the uterine muscle tissue.
Hysterectomy involves the removal of the entire uterus by coloscopy or surgery (either abdominal surgery or via a vaginal approach).
This treatment modality definitively eliminates the fibroids but both hospital stay and convalescence period are long. And of course, hysterectomy abolishes the possibility of later pregnancy.
Embolisation: This uterus-sparing procedure is performed with mild local anaesthesia and requires a hospital stay of approximately two days. Postoperative pain is managed with various drugs or by means of a small pump device with which the patient herself can control the dose administered according to her degree of pain. With a fast recovery, normal lifestyle can be resumed within one to two weeks. Embolisation does not compromise fertility although the procedure is not at this time licensed for the correction of leiomyoma-related infertility.
Before the embolisation procedure, you will be given a comprehensive medical checkup.
- A full physical and gynaecological examination carried out by your gynaecologist.
- Imaging to gauge the number, size and location of the fibroids, carried out by a radiologist.
- A pre-treatment examination is required in order to determine the most suitable anaesthesia and pain management modalities.
During the procedure: the embolisation procedure is carried out by an interventional radiologist who is specially trained in navigation through vessels and treatment via a radiological approach. You will be given drugs to control pain, but you will remain conscious throughout the procedure. The radiologist will insert a small plastic tube, known as a catheter, into an artery in the groin. With X-ray monitoring, the catheter is advanced until it reaches the uterine artery where small particles, each the size of a grain of sand, are injected into the vessels supplying the fibroids. This blocks the blood supply so that the fibroids shrink and the symptoms are attenuated.
After the procedure: you will remain in the hospital for one or two days for the management of postoperative pain. You will be able to return to work after 7 to 10 days. You may experience a low fever and mild fatigue in the days following the procedure. Bleeding may also occur in the following months. The fibroids may be expelled spontaneously, although this is rare. Your interventional radiologist and gynaecologist will be working closely together to follow up with you after the procedure. Follow-up details vary, but you will be asked to return for checkups one and six months after embolisation. An ultrasound scan or an MRI examination will be completed between three and six months following embolisation treatment. In any event, you should notify your physician about any abnormality you notice after embolisation.
"The catheter is advanced until it reaches the uterine artery where microspheres, each the size of a grain of sand, are injected into the vessels supplying the fibroids. This blocks the blood supply so that the fibroids shrink and the symptoms are attenuated."